Nelly Elwany1, Mahmoud Hassan Eid2, Amr A. Badreldin3 and Samy Elwany4*
Assistant professor, University of Kentucky College of Dentistry, USA
Assistant lecturer of Otolaryngology, Faculty of Medicine, Suez Canal University, Ismailia, Egypt
Doctoral Candidate, School of Dentistry, University of California Los Angeles, USA
Professor, Faculty of Medicine, Alexandria University, Egypt
Received: 06 January 2024; Accepted: 21 January 2024; Published: 28 January 2024
Citation: Elwany Nelly, Eid Mahmoud Hassan, Badreldin Amr A. and Elwany Samy. “Serious Deep Neck Infection as a Complication of Mandibular Dental Implant” J Oral Dis Treat (2024):101. DOI: 10.59462/JODT.1.1.101
Copyright: © 2024 Samy Elwany. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: Dental implantology is gaining great popularity for the treatment of partial or total edentulism. There are several potential complications related to dental implant surgery. We are herein reporting a case of life-threatening deep neck space infection following mandibular dental implant. To our knowledge, only three such similar cases were reported in the literature.
Case presentation: A 41-year-old female patient presented with rapidly progressive tender upper neck swelling of 4-day duration following mandibular left canine dental implant. Computed tomography of the neck showed evidence of a big inflammatory collection in the submandibular region and floor of the mouth. The patient underwent successful surgical drainage with removal of the implant and discharged on the 10th postoperative day.
Conclusions: Upper deep neck infection may occur following mandibular dental implant procedure. Prompt management should be instituted. Airway should be secured, pus should be drained, and the offending implant should be removed.
Dental implant • Mandibular • Deep neck space infection
The introduction of dental implants as an option for partially and fully edentulous patients has revolutionized dental treatment. The implant becomes osseointegrated within few months, allowing it to withstand chewing and biting forces, similar to natural tooth function. A common indication for undergoing a dental implant procedure is replacement of a missing tooth/teeth. Complications of the implant procedure may occur during or after the procedure.
Deep neck infection represents a challenging problem for many reasons, the anatomy of the deep neck spaces is highly complex, the deep neck spaces are surrounded by a network of vital structures that may become involved in the inflammatory process, and the airway may be at risk in patients especially when the inflammation is rapidly progressing. In addition, certain deep neck spaces may extend to other portions of the body (e.g., mediastinum).
Prompt control of deep upper neck infection is essential to avoid the risk of respiratory distress and stridor. The airway should be secured, pus should be drained, and the implant should be removed. Coordination between otorhinolaryngologists anesthetist, and the dentist is important in such cases.
Submandibular space infection following dental implantation is uncommon complication. To our knowledge, only three cases were reported in the literature with deep neck space infection following dental implantation.
Case Presentation
A 41-year-old female patient with no history of chronic illnesses presented to our hospital with diffuse neck swelling of 4 days duration following dental implant procedure done for the left mandibular canine tooth. The neck swelling is of acute onset, rapidly progressive course, with no improvement on medical treatment. She gave history of an implant done for the right mandibular canine tooth 1 year ago.
On examination, the patient was feverish. She had hoarseness and respiratory distress. The neck swelling was tense, tender with erythematous overlying skin involving the submental, bilateral submandibular regions down to the level of the thyroid cartilage (Figure 1). Oropharyngeal exam showed evidence of trismus, sublingual edema and pus oozing from the margin of an implant in the left mandibular canine tooth.
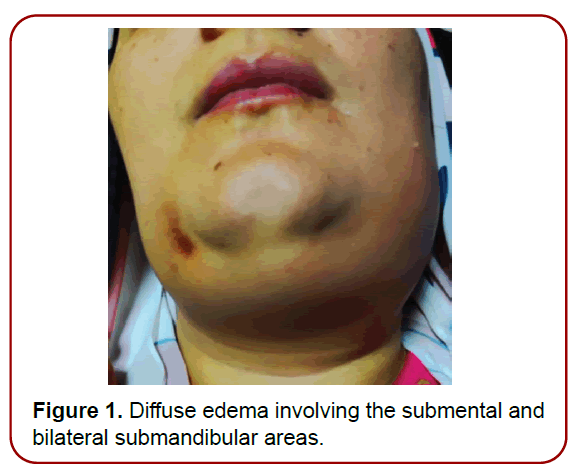
Figure 1. Diffuse edema involving the submental and bilateral submandibular areas.
Diagnostic Assessment
Complete blood picture showed leukocytosis. Computed tomography of the neck showed air foci in the submental, bilateral submandibular and anterior visceral neck spaces (Figure 2-4). Flexible fiberoptic assessment of the upper airway showed laryngeal edema.
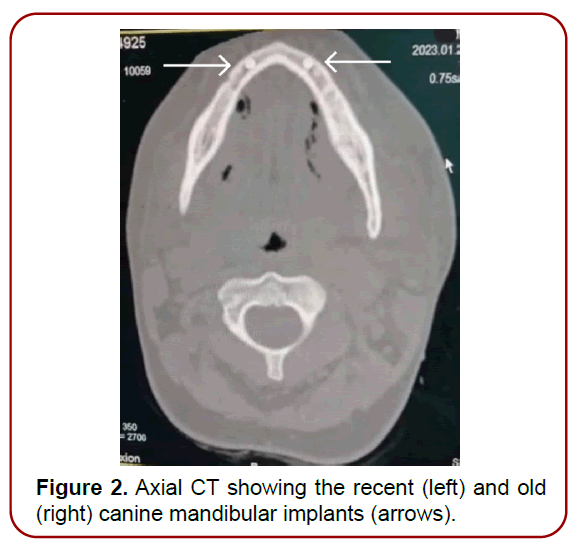
Figure 2. Axial CT showing the recent (left) and old (right) canine mandibular implants (arrows).
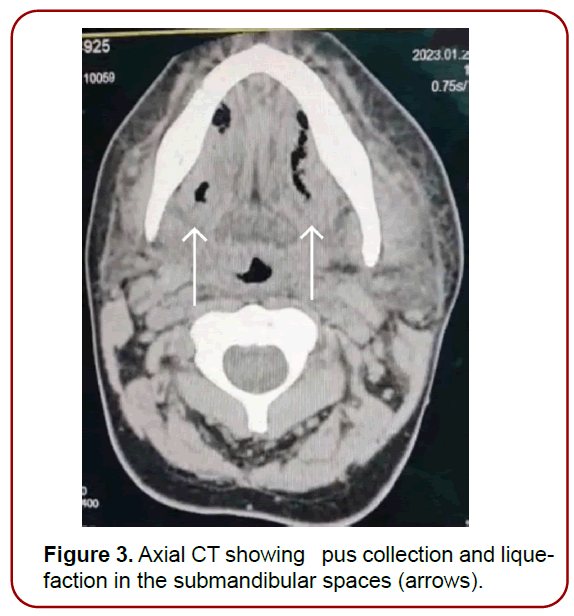
Figure 3. Axial CT showing pus collection and liquefaction in the submandibular spaces (arrows).
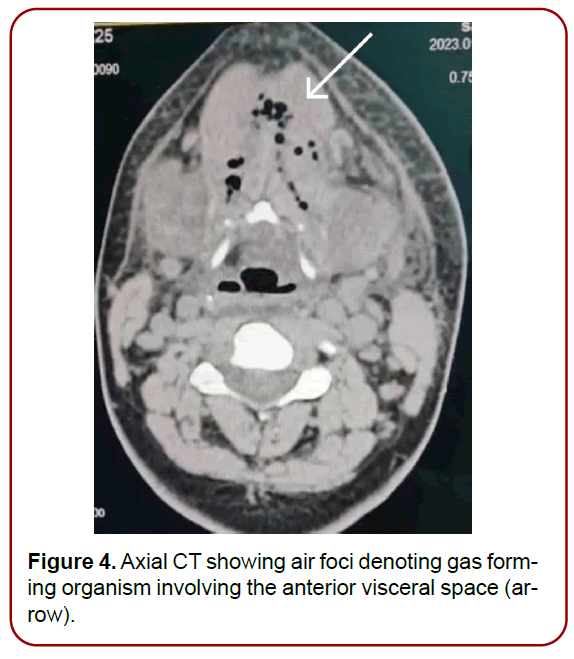
Figure 4. Axial CT showing air foci denoting gas forming organism involving the anterior visceral space (arrow).
Therapeutic Intervention
Antiedematous measures, IV fluids and IV antibiotics were started in the emergency room.
Planning for surgery was done between the otorhinolaryngologist, anesthesiologist for adequate intraoperative airway management and the dentist for infected implant removal.
Successful awake flexible fiberoptic nasotracheal intubation was done followed by surgical evacuation of the neck abscess which involved the submental, sublingual, bilateral submandibular spaces and anterior visceral space (Figure 5). Samples of pus were sent for culture and sensitivity. The infected implant was finally removed.
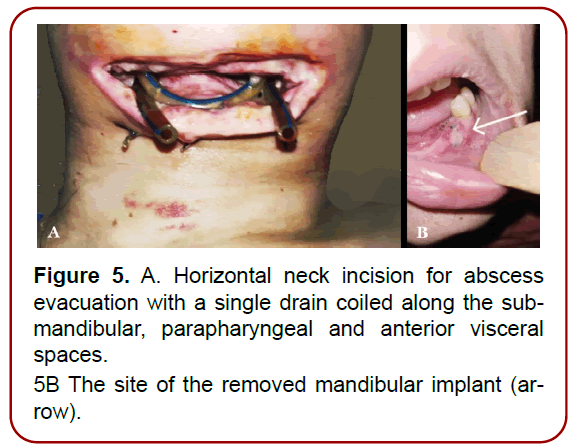
Figure 5. A. Horizontal neck incision for abscess
evacuation with a single drain coiled along the submandibular,
parapharyngeal and anterior visceral
spaces.
5B The site of the removed mandibular implant (arrow).
Outcome and follow-up
The patient was admitted to the intensive care unit for 5 days until resolution of the airway and sublingual edema. Antibiotics were given; based on the results of culture which showed staph aureus and peptostreptococci being sensitive to clindamycin and ceftriaxone.
The patient was extubated on the 4th postoperative day. Computed tomography of the neck was done 2 days postoperatively and it showed successful drainage of the abscess (Figure 6). The patient was discharged on the 10th postoperative day.
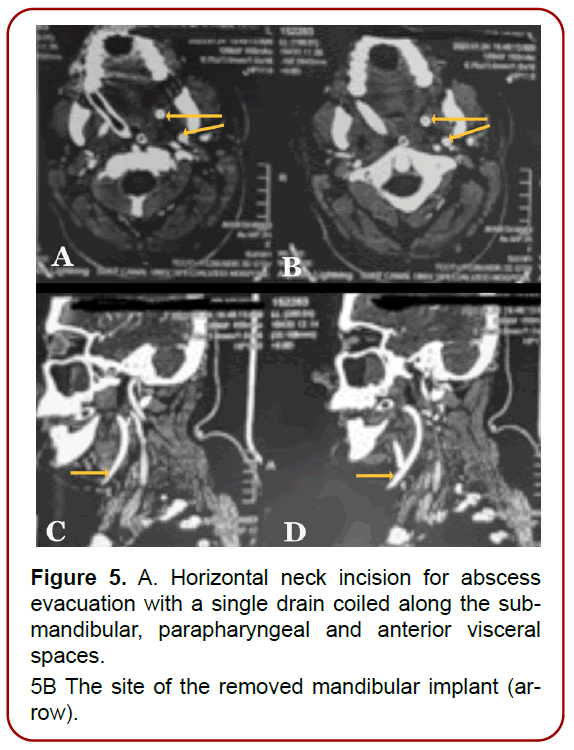
Figure 5. A. Horizontal neck incision for abscess
evacuation with a single drain coiled along the submandibular,
parapharyngeal and anterior visceral
spaces.
5B The site of the removed mandibular implant (arrow).
Informed Consent
The patient was informed with every step taken in the diagnostic assessment and was convinced that the physician’s plan in diagnosing and further management of her case would be helpful.
Submandibular space infection is considered a lifethreatening complication with the most common etiology being odontogenic in adults.
The cause of this massive abscess was apparently related to the perforation of the lingual mandibular cortex and consequent instability of the implant. This represented the gateway of the infection, with successive dissemination to the other spaces. In cases of odontogenic deep neck space infection, the culprit tooth or implant as in our case should be removed.
In one of the previously reported cases, the implant wasn’t removed after evacuation of the abscess. Later, the condition progressed for mediastinal extension of the neck infection and another extensive surgery was needed with longer hospital stay (27 days) [1-3].
In a second case, that was reported in 2019, the infected implant was removed but surgical intervention was delayed, which resulted in worsening and extension of the neck infection. Later on, the patient underwent two surgeries for evacuation of the neck abscess and he developed mediastinal complications with very long hospital stay (49 days) [4-7].
Based on the literature review and our experience in the present case, it is recommended to remove the offending implant and to carefully and promptly secure the airway and manage the neck infection as early as possible.
Deep neck space infections have high risk of airway and mediastinal complications if not properly managed. Early multidisciplinary management is crucial in these cases. Endotracheal intubation of these patients might be difficult, and the anesthesiologist should be prepared for flexible fiberoptic nasotracheal intubation. The offending implant should be removed, and the abscesses should be evacuated. Culture-directed intravenous antibiotics are needed and the patient should be kept under observation for any respiratory distress or stridor.
Ethics Approval and Consent to Participate
Study was approved by the local ethics committee (Faculty of Medicine Suez Canal University (Date of approval – may2023).
Consent to Participate
Written consent was obtained from study participant and she has been informed about the procedures to be done and the expected results.
Consent for Publication
Written Consent for study publication was obtained from the study participant.
Authors’ Contributions
ME did the neck surgery and contributed to the section of therapeutic intervention. NE analyzed and interpreted the patient data and wrote the discussion. AB wrote the patient history and clinical findings and did the literature review. SE read and approved the final manuscript.